The dose of LANTUS should be adjusted according to blood glucose measurements. The dosage of
LANTUS should be individualized under the supervision of a healthcare provider in accordance with
the needs of the patient.
2.3 Converting to LANTUS from other insulin therapies
If changing from a treatment regimen with an intermediate- or long-acting insulin to a regimen with
LANTUS, the amount and timing of shorter-acting insulins and doses of any oral anti-diabetic drugs
may need to be adjusted.
• If transferring patients from once-daily NPH insulin to once-daily LANTUS, the recommended initial
LANTUS dose is the same as the dose of NPH that is being discontinued.
• If transferring patients from twice-daily NPH insulin to once-daily LANTUS, the recommended initial
LANTUS dose is 80% of the total NPH dose that is being discontinued. This dose reduction will
lower the likelihood of hypoglycemia [
see Warnings and Precautions (5.3)].
3. DOSAGE FORMS AND STRENGTHS
LANTUS solution for injection 100 Units per mL is available as:
- 10 mL Vial (1000 Units/10 mL)
- 3 mL Cartridge systems for use only in OptiClik
®
(300 Units/3 mL)
- 3 mL SoloStar
®
disposable insulin device (300 Units/3 mL)
4. CONTRAINDICATIONS
LANTUS is contraindicated in patients with hypersensitivity to LANTUS or one of its excipients.
5. WARNINGS AND PRECAUTIONS
5.1 Dosage adjustment and monitoring
Glucose monitoring is essential for all patients receiving insulin therapy. Changes to an insulin regimen
should be made cautiously and only under medical supervision.
Changes in insulin strength, manufacturer, type, or method of administration may result in the need for
a change in insulin dose or an adjustment in concomitant oral anti-diabetic treatment.
As with all insulin preparations, the time course of action for LANTUS may vary in different individuals
or at different times in the same individual and is dependent on many conditions, including the local
blood supply, local temperature, and physical activity.
5.2 Administration
Do not administer LANTUS intravenously or via an insulin pump. The intended duration of activity of
LANTUS is dependent on injection into subcutaneous tissue
Intravenous administration of the usual subcutaneous dose could result in severe hypoglycemia
[see
Warnings and Precautions (5.3)]
.
Do not dilute or mix LANTUS with any other insulin or solution. If LANTUS is diluted or mixed, the
solution may become cloudy, and the pharmacokinetic or pharmacodynamic profile (e.g., onset of
action, time to peak effect) of LANTUS and the mixed insulin may be altered in an unpredictable
manner. When LANTUS and regular human insulin were mixed immediately before injection in dogs,
a delayed onset of action and a delayed time to maximum effect for regular human insulin was
observed. The total bioavailability of the mixture was also slightly decreased compared to separate
injections of LANTUS and regular human insulin. The relevance of these observations in dogs to
humans is unknown.
Do not share disposable or reusable insulin devices or needles between patients, because doing so
carries a risk for transmission of blood-borne pathogens.
5.3 Hypoglycemia
Hypoglycemia is the most common adverse reaction of insulin, including LANTUS. The risk of
hypoglycemia increases with intensive glycemic control. Patients must be educated to recognize and
manage hypoglycemia. Severe hypoglycemia can lead to unconsciousness or convulsions and may
result in temporary or permanent impairment of brain function or death. Severe hypoglycemia requiring
the assistance of another person or parenteral glucose infusion or glucagon administration has been
observed in clinical trials with insulin, including trials with LANTUS.
The timing of hypoglycemia usually reflects the time-action profile of the administered insulin
formulations. Other factors such as changes in food intake (e.g., amount of food or timing of meals),
exercise, and concomitant medications may also alter the risk of hypoglycemia [
See Drug Interactions
(7)].
The prolonged effect of subcutaneous LANTUS may delay recovery from hypoglycemia. Patients being
switched from twice daily NPH insulin to once-daily LANTUS should have their initial LANTUS dose
reduced by 20% from the previous total daily NPH dose to reduce the risk of hypoglycemia
[see Dosage
and Administration (2.3)].
As with all insulins, use caution in patients with hypoglycemia unawareness and in patients who may
be predisposed to hypoglycemia (e.g., the pediatric population and patients who fast or have erratic
food intake). The patient’s ability to concentrate and react may be impaired as a result of hypoglycemia.
This may present a risk in situations where these abilities are especially important, such as driving or
operating other machinery.
Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions,
such as longstanding diabetes, diabetic neuropathy, use of medications such as beta-blockers, or
intensified glycemic control. These situations may result in severe hypoglycemia (and, possibly, loss
of consciousness) prior to the patient’s awareness of hypoglycemia.
5.4 Hypersensitivity and allergic reactions
Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulin products,
including LANTUS.
5.5 Renal impairment
Due to its long duration of action, Lantus is not recommended during periods of rapidly declining renal
function because of the risk for prolonged hypoglycemia.
Although studies have not been performed in patients with diabetes and renal impairment, a reduction
in the LANTUS dose may be required in patients with renal impairment because of reduced insulin
metabolism, similar to observations found with other insulins.
[See Clinical Pharmacology (12.3)].
5.6 Hepatic impairment
Due to its long duration of action, Lantus is not recommended during periods of rapidly declining hepatic
function because of the risk for prolonged hypoglycemia.
Although studies have not been performed in patients with diabetes and hepatic impairment, a reduction
in the LANTUS dose may be required in patients with hepatic impairment because of reduced capacity
for gluconeogenesis and reduced insulin metabolism, similar to observations found with other insulins.
[See Clinical Pharmacology (12.3)].
5.7 Drug interactions
Some medications may alter insulin requirements and subsequently increase the risk for hypoglycemia
or hyperglycemia
[See Drug Interactions (7)].
6. ADVERSE REACTIONS
The following adverse reactions are discussed elsewhere:
• Hypoglycemia
[See Warnings and Precautions (5.3)]
• Hypersensitivity and allergic reactions [See Warnings and Precautions (5.4)]
6.1 Clinical trial experience
Because clinical trials are conducted under widely varying designs, the adverse reaction rates reported
in one clinical trial may not be easily compared to those rates reported in another clinical trial, and may
not reflect the rates actually observed in clinical practice.
The frequencies of treatment-emergent adverse events during LANTUS clinical trials in patients with
type 1 diabetes mellitus and type 2 diabetes mellitus are listed in the tables below.
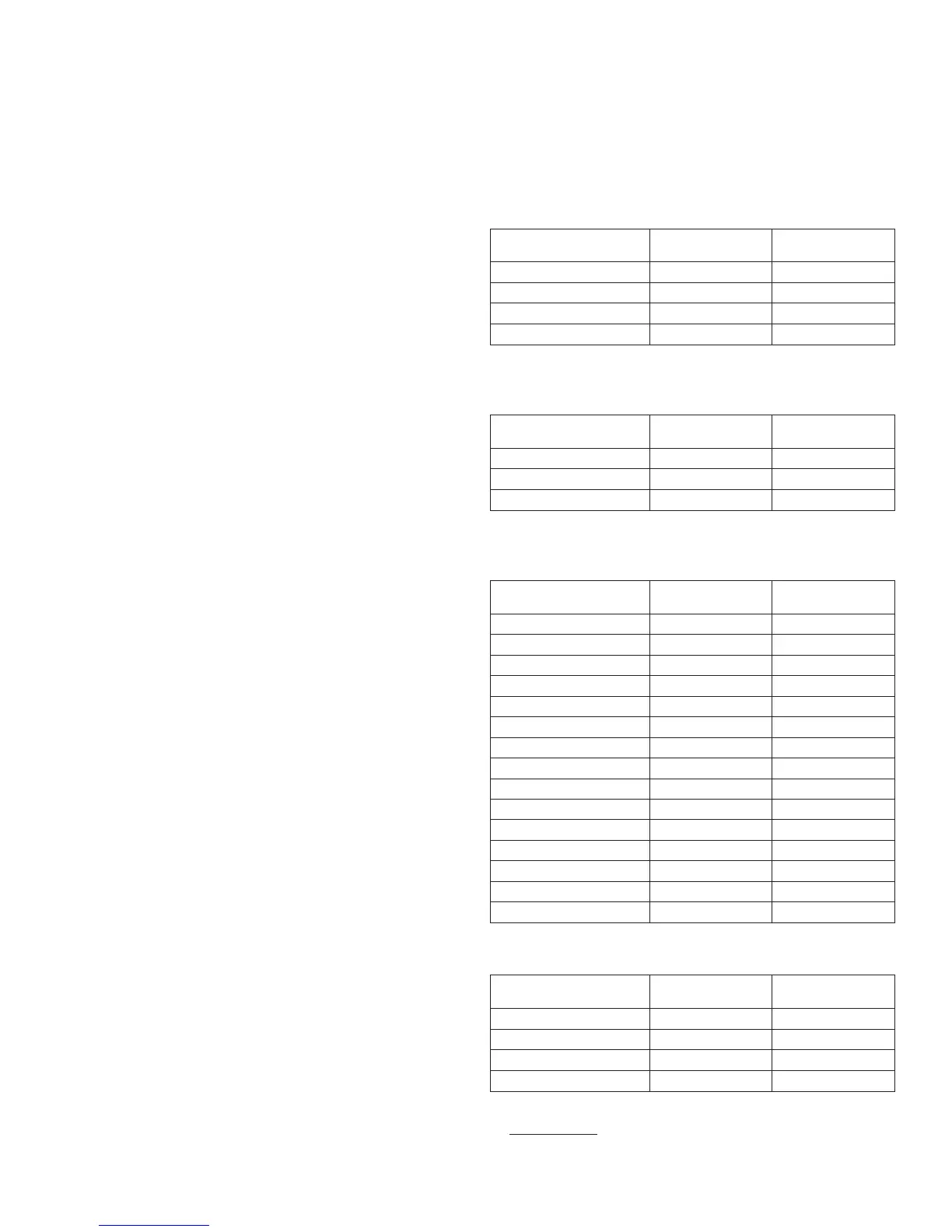
Table 1: Treatment –emergent adverse events in pooled clinical trials up to 28 weeks
duration in adults with type 1 diabetes (adverse events with frequency ≥ 5%)
LANTUS, %
(n=1257)
NPH, %
(n=1070)
Upper respiratory tract infection 22.4 23.1
Infection
*
9.4 10.3
Accidental injury 5.7 6.4
Headache 5.5 4.7
*Body System not Specified
Table 2: Treatment –emergent adverse events in pooled clinical trials up to 1 year
duration in adults with type 2 diabetes (adverse events with frequency ≥ 5%)
LANTUS, %
(n=849)
NPH, %
(n=714)
Upper respiratory tract infection 11.4 13.3
Infection
*
10.4 11.6
Retinal vascular disorder 5.8 7.4
*Body System not Specified
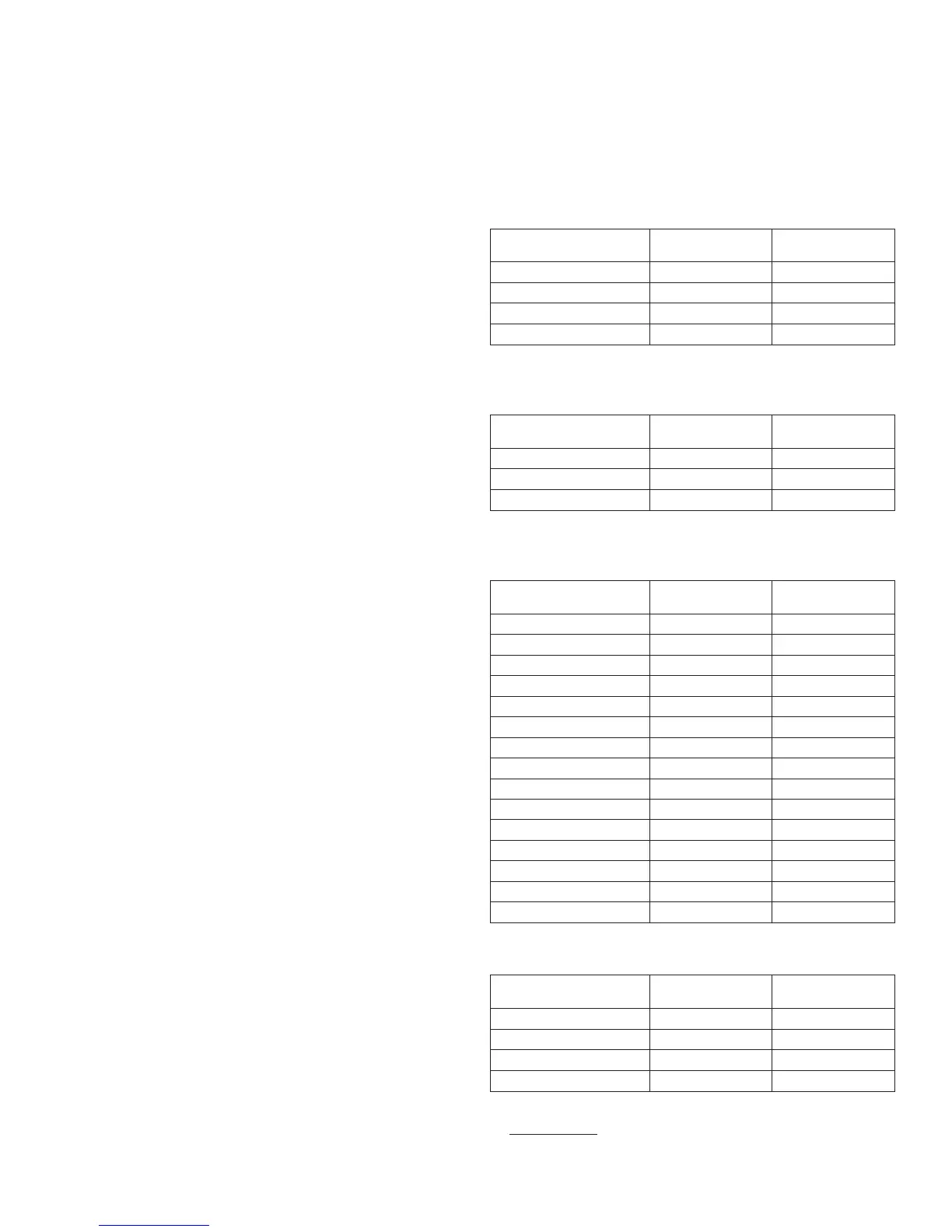
Table 3: Treatment –emergent adverse events in a 5-year trial of adults with type 2
diabetes (adverse events with frequency ≥ 10%)
LANTUS, %
(n=514)
NPH, %
(n=503)
Upper respiratory tract infection 29.0 33.6
Edema peripheral 20.0 22.7
Hypertension 19.6 18.9
Influenza 18.7 19.5
Sinusitis 18.5 17.9
Cataract 18.1 15.9
Bronchitis 15.2 14.1
Arthralgia 14.2 16.1
Pain in extremity 13.0 13.1
Back pain 12.8 12.3
Cough 12.1 7.4
Urinary tract infection 10.7 10.1
Diarrhea 10.7 10.3
Depression 10.5 9.7
Headache 10.3 9.3
Table 4: Treatment –emergent adverse events in a 28-week clinical trial of children and
adolescents with type 1 diabetes (adverse events with frequency ≥ 5%)
LANTUS, %
(n=174)
NPH, %
(n=175)
Infection
*
13.8 17.7
Upper respiratory tract infection 13.8 16.0
Pharyngitis 7.5 8.6
Rhinitis 5.2 5.1
*Body System not Specified
•
Severe Hypoglycemia
Hypoglycemia is the most commonly observed adverse reaction in patients using insulin, including
LANTUS
[See Warnings and Precautions (5.3)]. Tables 5 and 6 summarize the incidence of severe
hypoglycemia in the LANTUS individual clinical trials. Severe symptomatic hypoglycemia was defined
2

 Loading...
Loading...