6
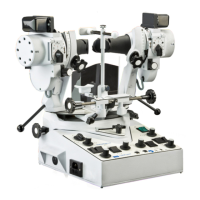
Synoptophore Instructions
9. The subjective angle and abnormal
retinal correspondence.
The subjective angle is found by instructing the
patient to move the handles (108) himself until the
two pictures are superimposed. If this angle is the
same as the objective angle, when small pictures
are used, the retinal correspondence is normal.
If, however, the angles differ, the retinal
correspondence is abnormal and the difference
b
etween the two is the angle of anomaly. These
measurements are made with the patient’s
prescribed correction; the appropriate lenses are
fitted into lens holders (118). The patient is then
measured without corrective lenses.
10. Side movements.
Lateral movements are valuable as a test of fusion
and as an orthoptic exercise. With a pair of slides
from the fusion range in the slide carriers and the
tubes set at an angle of deviation, the two tube
locking controls (121) are turned outwards. The
central lock (122) must be released. The tubes are
then moved side to side and the patient is
instructed to follow the movements of the pictures.
11. Vergences.
Horizontal vergences are measured on the scale
(119) which is engraved ‘ADD’ (Adduction - the
uniocular movement of the eye horizontally
INwards) and ‘ABD’ (Abduction - the uniocular
movement of the eye horizontally OUTwards).
Set the tubes at the angle of deviation and the scale
(119) at whichever zero mark is appropriate. A pair
of fusion slides must be used in the slide carriers.
Tighten the two tube locking controls (121) and
engage the central lock (122). Slowly rotate one or
both controls (121) whereupon the tubes will be
converged or diverged, according to the
requirements. The angle through which fusional
vergence is held by the patient is indicated on
scale (119) and the point where the pictures
‘break’, fusion is no longer maintained.
Vertical vergences are measured by rotating one
or other of the elevation and depression controls
(115). In both cases the corneal reflections should
be kept under observation.
12. Heterophoria.
Examination and measurement of cyclophoria is
possible with the Synoptophore by means of the
rotating slide carriers operated by controls (113).
Each carrier rotates 20˚ on either side of zero. The
phoria is indicated on scales (112).
Hyperphoria is measured on scales (110) in prism
dioptres, for the slide carriers move tangentially
up and down by the action of controls (111).
13. Dimming rheostats.
A
rotary rheostat is in circuit with each of the 6V.
slide illumination lamps. By means of the controls
(130) these rheostats reduce the intensity of the
light as required. In certain post-operative cases it
is desirable to lesson the light reaching the
patient’s eye, whilst when treating amblyopes it
may be necessary to reduce the illumination in
front of the good eye and maintain the maximum
light in front of the amblyopic eye.
14. Hand flashing switches.
The two buttons (129) operate micro-switches,
one of which is in circuit with each of the 6V.
lamps. One use has already been described in
section 5. A further use is to stimulate a
suppressing eye by rapid flashing.
15. Auxiliary lens holders.
The two lens holders (118) fitted into the
eyepieces are used to carry additional lenses,
when required.
16. Slide ejectors.
The slide ejectors (117) can be used to make the
slides ‘jump’ and therefore stimulate a
suppressing eye.
17. Promoting an after-image
(Models 2001and 2002 only).
The after-image device consists of two high
intensity light sources each containing a 12V. lamp
and a condensing lens. Supplied with the
Synoptophore are two special slides, S.3 and S.4,
one consisting of a vertical white slit, with a red
central fixation point on a black background and
the other a horizontal slit also with red spot. These
slides are inserted into the carriers with the matt
surface inwards, i.e. towards the patient. The
opal defusing screens must be swivelled down-
wards out of the optical pathway by rotating the
black plastic control levers (123) situated
immediately below the latch of the lamphousing.
This allows more light to pass through the slide
and thus a stronger after-image is produced. The
selector switch (131) is turned clockwise to the
first position ‘R’, and the mains switch (124) is
turned on. Instruct the patient to fix the red spot
and ensure that his fixation remains steady for
a period of some 7 to 10 seconds. Turn the
selector switch clockwise to the next stop, which
is an ‘off’ position, remove the right eye slide
and swivel back the diffusing screen. Then turn
the selector switch clockwise to the next position
‘L’ and ask the patient to fix the red spot for the
prescribed time. Finally, turn the switch still
further to one of the ‘off’ positions, whilst you
remove the left eye slide and swivel back the
diffusing screen.
 Loading...
Loading...