3
subsequent to the placement of the device. FDA recommends that implanting physicians and clinicians
responsible for the ongoing care of patients with retrievable IVC filters consider removing the filter as
soon as protection from PE is no longer needed. FDA encourages all physicians involved in the treatment
and follow-up of IVC filter recipients to consider the risks and benefits of filter removal for each patient.
See Reporting Standards for Inferior Vena Caval Filter Placement and Patient Follow-up: Supplement
for Temporary and Retrievable/Optional Filters. Millward, S., et al.: J. Vasc Interv Radiol 2005; 16:441-
443; Recommended Reporting Standards for Vena Cava Filter Placement and Patient Follow-up. The
Participants in the Vena Caval Filter Consensus Conference: J Vasc Inter Radiol 2003; 14:S427-S432;
Guidelines for the Use of Retrievable and Convertible Vena Cava Filters: Report from the Society of
Interventional Radiology Multidisciplinary Consensus Conference. Kaufman, J., et al.: J Vasc Interv Radiol
2006; 17:449-459.
G. Potential Complications
Procedures requiring percutaneous interventional techniques should not be attempted by physicians unfamiliar
with the possible complications. Complications may occur at any time during or after the procedure.
Possible complications include, but are not limited to, the following:
• Movement, migration or tilt of the filter are known complications of vena cava filters. Migration of filters to the
heart or lungs has been reported. There have also been reports of caudal migration of the filter. Migration may
be caused by placement in IVCs with diameters exceeding the appropriate labeled dimensions specified in this
IFU. Migration may also be caused by improper deployment, deployment into clots and/or dislodgement due to
large clot burdens.
• Filter fractures are a known complication of vena cava filters. There have been some reports of serious
pulmonary and cardiac complications with vena cava filters requiring the retrieval of the fragment utilizing
endovascular and/or surgical techniques.
• Detachment of components
• Perforation or other acute or chronic damage of the IVC wall.
• Acute or recurrent pulmonary embolism. This has been reported despite filter usage. It is not known if thrombi
passed through the filter, or originated from superior or collateral vessels.
• Deep vein thrombosis
• Caval thrombosis/occlusion
• Extravasation of contrast material at time of venacavogram.
• Air embolism
• Hematoma or nerve injury at the puncture site or subsequent retrieval site.
• Hemorrhage
• Restriction of blood flow
• Occlusion of small vessels
• Distal embolization
• Infection
• Intimal tear
• Stenosis at implant site.
• Failure of filter expansion/incomplete expansion.
• Insertion site thrombosis
• Filter malposition
• Vessel injury
• Arteriovenous fistula
• Back or abdominal pain
• Filter tilt
• Hemothorax
• Organ injury
• Phlegmasia cerulea dolens
• Pneumothorax
• Postphlebitic syndrome
• Stroke
• Thrombophlebitis
• Venous ulceration
• Blood loss
• Guidewire entrapment
• Pain
All of the above complications may be associated with serious adverse events such as medical
intervention and/or death. There have been reports of complications including death, associated with the
use of vena cava filters in morbidly obese patients. The risk/benefit ratio of any of these complications
should be weighed against the inherent risk/benefit ratio for a patient who is at risk of pulmonary
embolism without intervention.
H. Clinical Experience
A single-arm, prospective, multi-center clinical study was conducted to assess the safety of the DENALI
®
Filter as
both a permanent and retrievable device. Clinical Success of Placement (CSP) was defined as freedom from
subsequent PE, filter embolization, caval occlusion, filter or procedure related death, insertion adverse events,
and technical failure of placement. The pre-established performance goal was that the lower bound of the 95%
confidence interval for the CSP was greater than 80%. Technical Success of Placement (TSP) was defined as
deployment of the filter such that the physician judged the location to be suitable to provide sufficient mechanical
protection against PE. Technical Success of Retrieval (TSR) was defined as retrieval of the filter such that the
entire filter was retrieved intact. Clinical Success of Retrieval (CSR) was defined as successful technical retrieval
of the filter without retrieval complications requiring intervention. Additionally, the secondary endpoints of recurrent
PE, new or worsening DVT, filter migration, filter fracture, penetration and tilt were assessed.
Two hundred (200) patients (126 males, 74 females) were enrolled at 21 investigational sites across the United
States. The mean age was 56.6±15.63 years (range 18 – 89 years). One hundred twenty-one (121) patients had
their filter successfully retrieved..
Of the 200 patients who underwent DENALI
®
Filter placement, 120 had active thromboembolic disease (the
presence of DVT or PE at the time of filter placement). Of these 120 patients, 66 had a contraindication
to anticoagulation, 9 had a complication related to the use of anticoagulant medication, 20 had a failure of
anticoagulation, and 25 had a filter placed without contraindication, complication or failure related to anticoagulant
medication. Eighty (80) patients without active thromboembolic disease (neither DVT nor PE at the time of filter
placement) were enrolled in the study.
Reasons for filter placement were as follows: Surgery (n=87, 43.5%), Trauma (n=41, 20.5%), Hypercoagulopathy
(n=44, 22%), Cancer (n=10, 5%), Stroke (n=3, 1.5%) and Other (n=15, 7.5%).
Ninety eight (98) patients completed a six month visit, sixty eight (68) patients completed a 12 month visit, fifty
three (53) patients completed an 18-month visit, and forty six (46) patients completed a 24 month visit. Four
patients were withdrawn from the study, twelve (12) were lost to follow up and twenty one (21) died from pre-
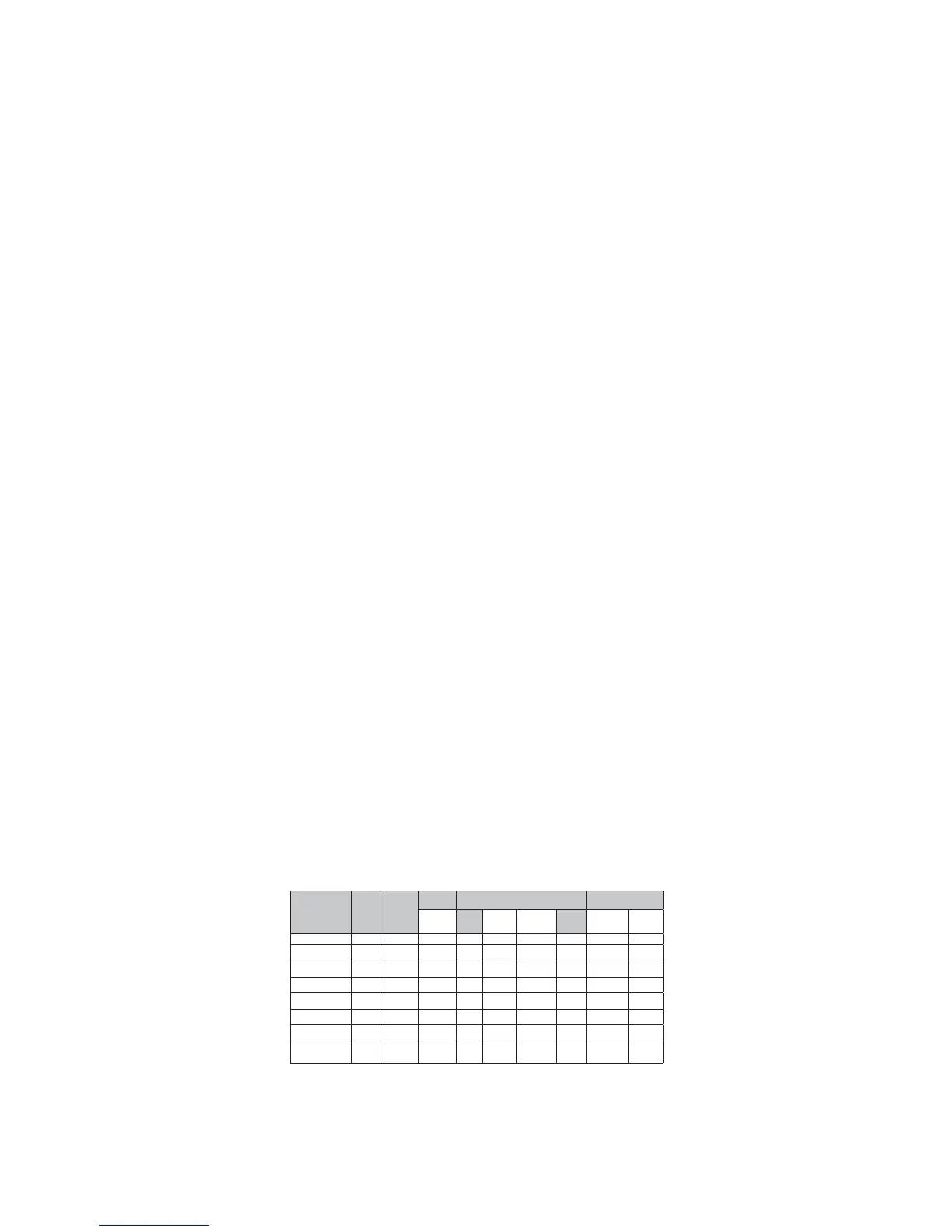
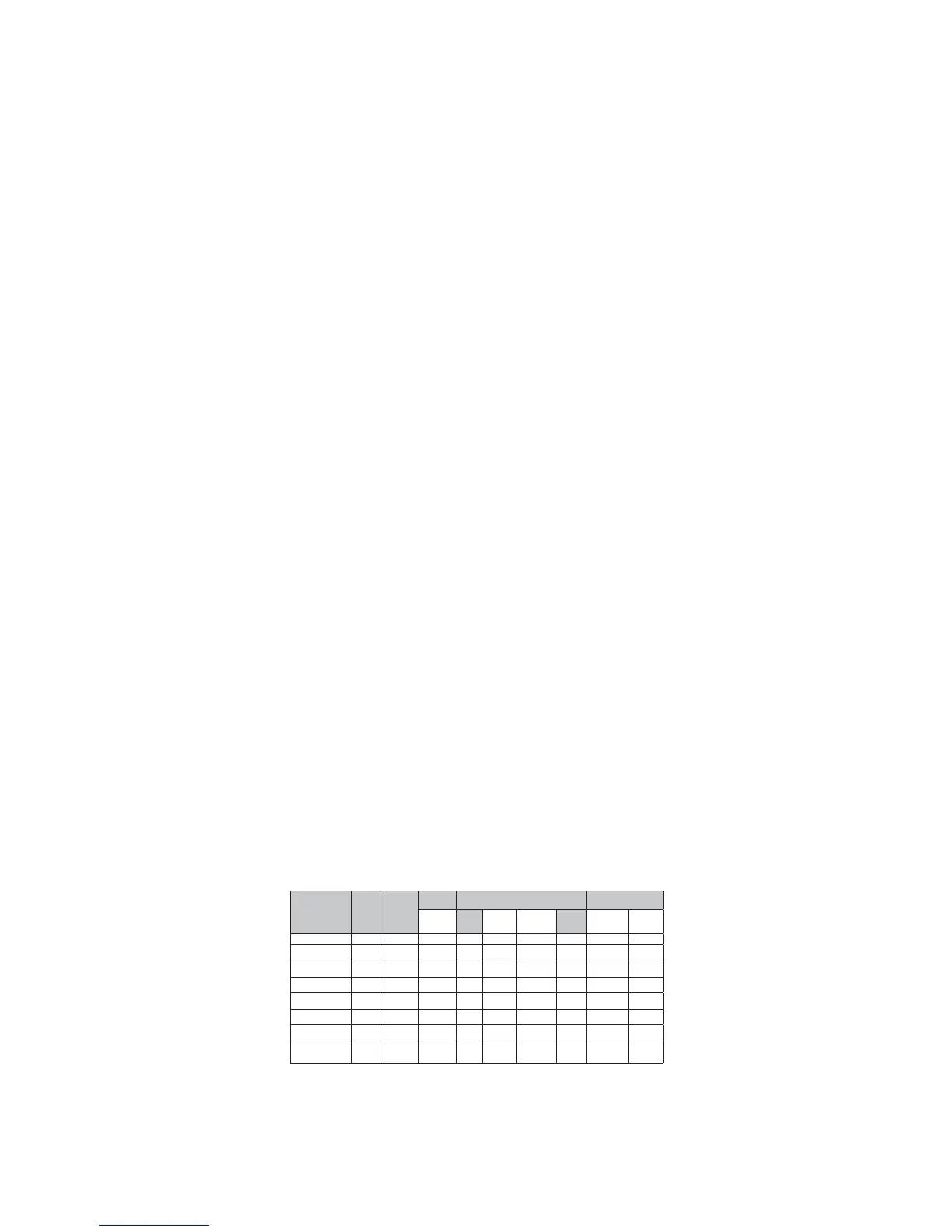
existing or inter-current conditions. Refer to the results sections for more details. Table 1 displays the completed
patient follow-up at each time point.
Table 1: Patient Accountability
1
5 subjects had their filter retrieved in 3M window and are considered “visit complete”; 1 eligible subject died in 3M window; 1 eligible subject was LTF in 3M window.
2
13 subjects had their filter retrieved in 6M window and are considered “visit complete”; 1 eligible subject died in 6M window; 2 retrieved in 6M window missed the 6M
visit; 2 eligible subjects were LTF in the 6M window; 2 eligible subjects were withdrawn in the 6M window.
3
4 subjects had their filter retrieved in 12M window and are considered “visit complete”; neither withdrawn subject was eligible for the 12M visit; 1 eligible subject died in
12M window; 1 eligible subject was LTF in 12M window.
4
1 eligible subject was LTF in 18M window.
5
2 subjects completed both the 24M visit and filter retrieval visit; 2 eligible subjects were LTF in the 24M window.
6
1 subject had an unsuccessful retrieval attempt but returned for a second attempt which was successful.
Results
CSP for the DENALI
®
Filter was 95.0% and the lower bound of the 95% confidence interval was 91.2%. It was
concluded that the performance goal was met. TSP for the DENALI
®
Filter was 99.5%. Mean placement procedure
time was 17.8 minutes and mean fluoroscopy time was 3.6 minutes. TSR for the DENALI
®
Filter was 97.6%. CSR
for the DENALI
®
Filter was 99.2%.
Eligible
for Visit
(N)
Visit
Complete
(N, %)
Reason Visit Not Completed
Events Occurring
Before Next Visit
Retrieved Death
Lost to
Follow-Up
Withdrawn
Missed
Visit
Migration Fracture
Baseline/ Implant 200 200 N/A 0 0 0 0 0 0
3 Months
1
165 157 (95%) 30 11 1 0 6 0 0
6 Months
2
130 112 (86%) 39 3 2 2 15 0 0
12 Months
3
77 71 (92%) 38 3 2 2 4 0 0
18 Months
4
54 53 (98%) 8 3 3 0 0 0 0
24 Months
5
48 46 (96%) 6 1 2 0 0 0 0
Retrieval
6
124 121 121 N/A N/A N/A N/A 0 0
30 Days
Post-
Retrieval
121 119 (98%) N/A N/A 2 N/A N/A N/A N/A
 Loading...
Loading...