GMK Sphere Calipered Kinematic Alignment Surgical Technique
20
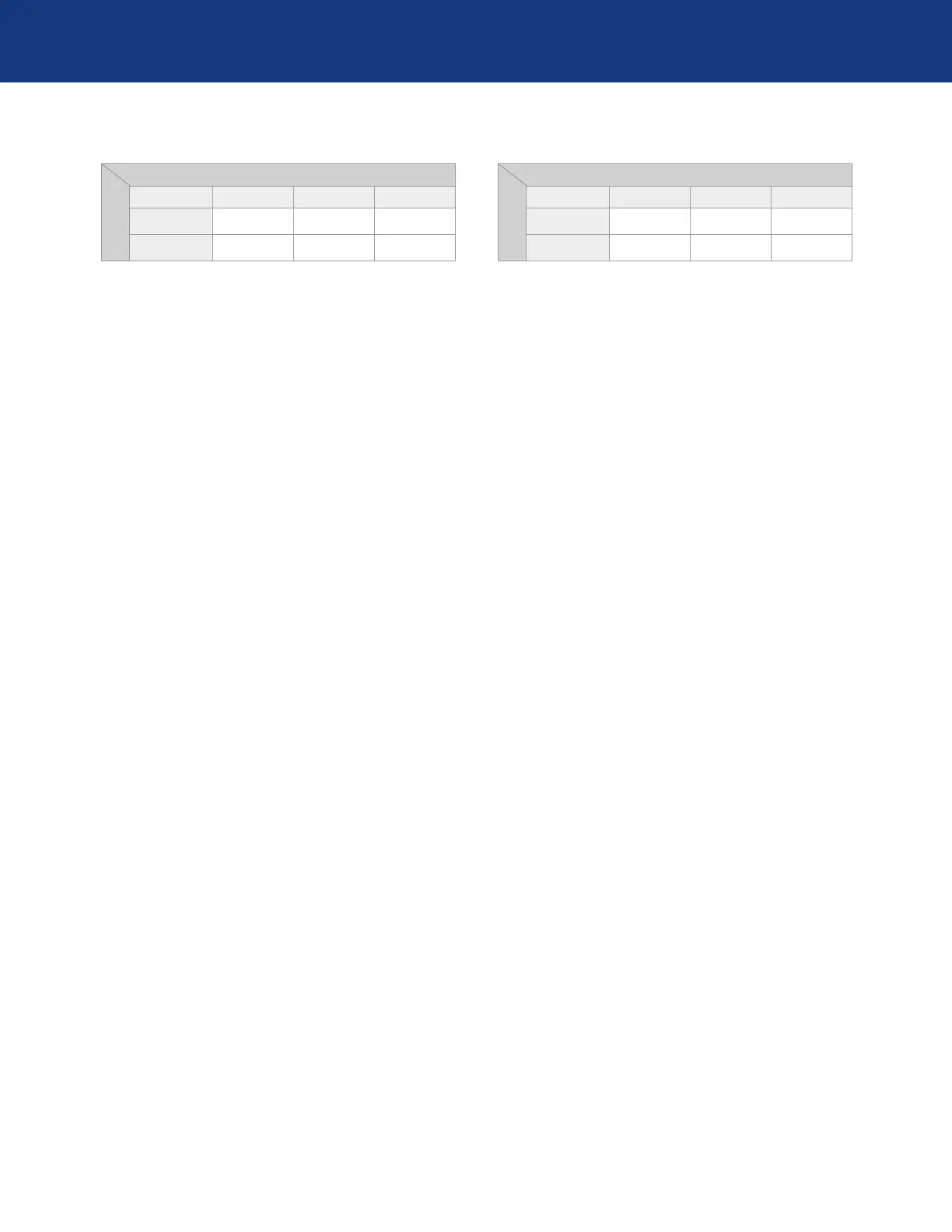
FLEXION
EXTENSION
Tight Ok Loose
Tight 1 2 3
OK 4 5 6
GMK SPHERE DECISION-TREE - FLEX INSERT
1. If the joint is tight both in extension and flexion recut
tibia and remove 1-2 mm more bone (or if possible
decrease the thickness of the articular surface)
2. If the joint is tight in extension and well balanced in
flexion:
•
Remove posterior femoral osteophytes.
•
Strip posterior capsule.
•
Insert trial component and gently manipulate knee
into extension.
•
Reassess.
•
Resect additional proximal tibial bone with decreased
posterior slope and increase the thickness of the
articular surface.
3. If the joint is tight in extension and loose in flexion:
•
Remove posterior osteophytes.
•
Strip posterior capsule.
•
Insert trial component and gently manipulate knee
into extension.
•
Reassess.
•
Resect an additional 2 mm from the distal femur and
use a 2-mm thicker liner. *
4. If the joint is well balanced in extension and tight in
flexion:
•
Confirm complete resection of the PCL.
•
Increase posterior slope.
5. If the joint is well balanced both in extension and flexion
no further modifications are necessary.
6. If the articulation is well balanced in extension and loose
in flexion:
•
If still loose in flexion reduce slope or resect 1 - 2
mm bone from distal femur and add thicker Sphere
CS insert.
•
Add thicker spacer and recheck knee extends fully.
•
Remove posterior osteophytes.
•
Strip posterior capsule.
•
Insert trial component and gently manipulate knee
into extension.
•
Reassess.
•
Resect additional proximal tibial bone with
decreased posterior slope and increase the
thickness of the articular surface.
* This approach requires the surgeon to accept
that raising the femoral joint line by 2 mm
violates the kinematic alignment goal of restoring
the native tibial-femoral articular surfaces
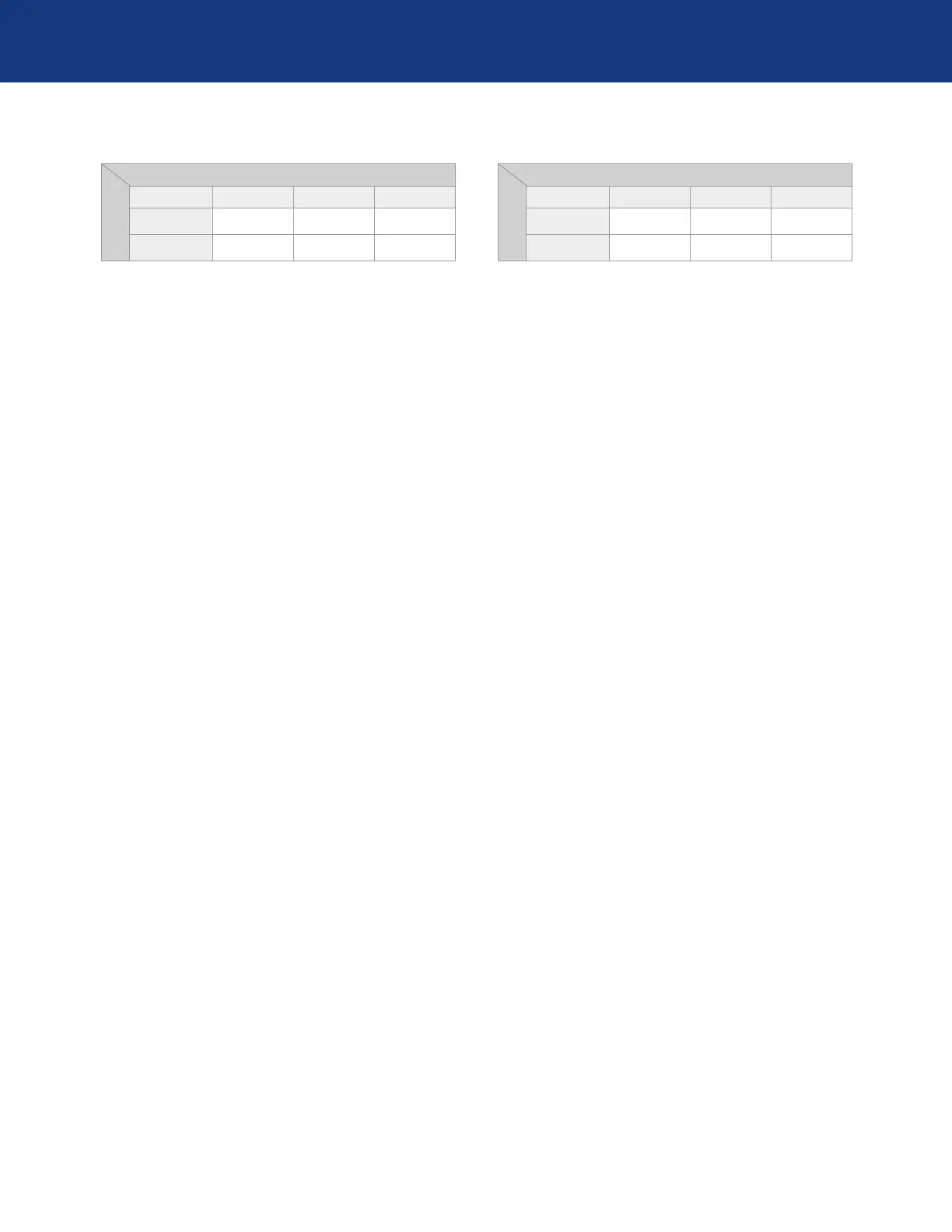
FLEXION
EXTENSION
Tight Ok Loose
Tight 1 2 3
OK 4 5 6
GMK SPHERE DECISION-TREE - CR INSERT
1. If the joint is tight both in extension and flexion recut
tibia and remove 1-2 mm more bone (or if possible
decrease the thickness of the articular surface)
2. If the joint is tight in extension and well balanced in
flexion:
•
Remove posterior osteophytes.
•
Strip posterior capsule.
•
Insert trial component and gently manipulate knee
into extension.
•
Reassess.
•
Resect additional proximal tibial bone with decreased
posterior slope and increase the thickness of the
articular surface.
3. If the joint is tight in extension and loose in flexion:
•
Remove posterior osteophytes.
•
Strip posterior capsule.
•
Insert trial component and gently manipulate knee
into extension.
•
Reassess.
•
Resect an additional 2 mm from the distal femur and
use a 2-mm thicker liner. *
4. If the joint is well balanced in extension and tight in
flexion, increase posterior slope until native A-P offset is
restored at 90° of flexion.
5. If the joint is well balanced both in extension and flexion
no further modifications are necessary.
6. If the articulation is well balanced in extension and loose
in flexion:
•
When knee does not fully extend check PCL tension.
•
When PCL is incompetent use Sphere Flex insert.
•
Add thicker spacer and recheck knee extends fully.
•
Remove posterior osteophytes.
•
Strip posterior capsule.
•
Insert trial component and gently manipulate knee
into extension.
•
Reassess
•
Resect additional proximal tibial bone with
decreased posterior slope and increase the
thickness of the articular surface.
* This approach requires the surgeon to accept
that raising the femoral joint line by 2 mm violates
the kinematic alignment goal of restoring the native
tibial-femoral articular surfaces
 Loading...
Loading...