Chapter 8: Oximetry
VS2000 Vital Signs Monitor Operation Manual 8-3
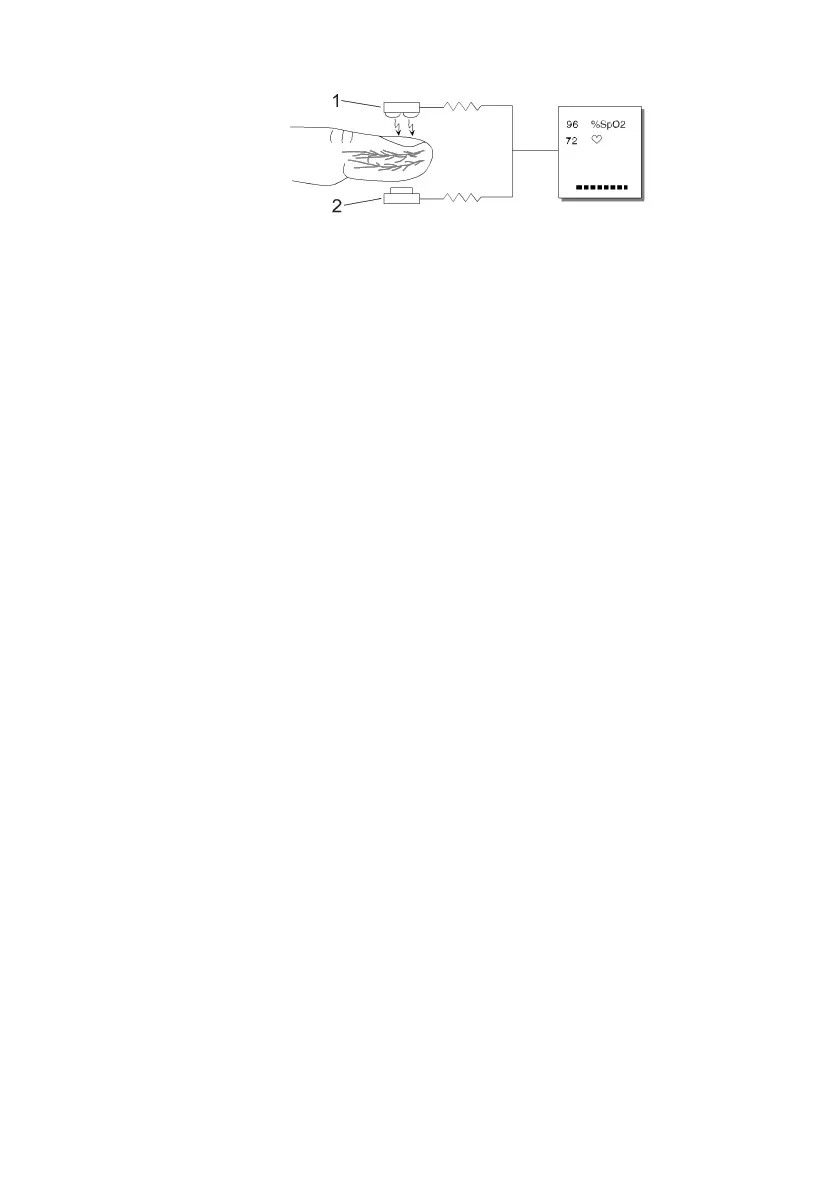
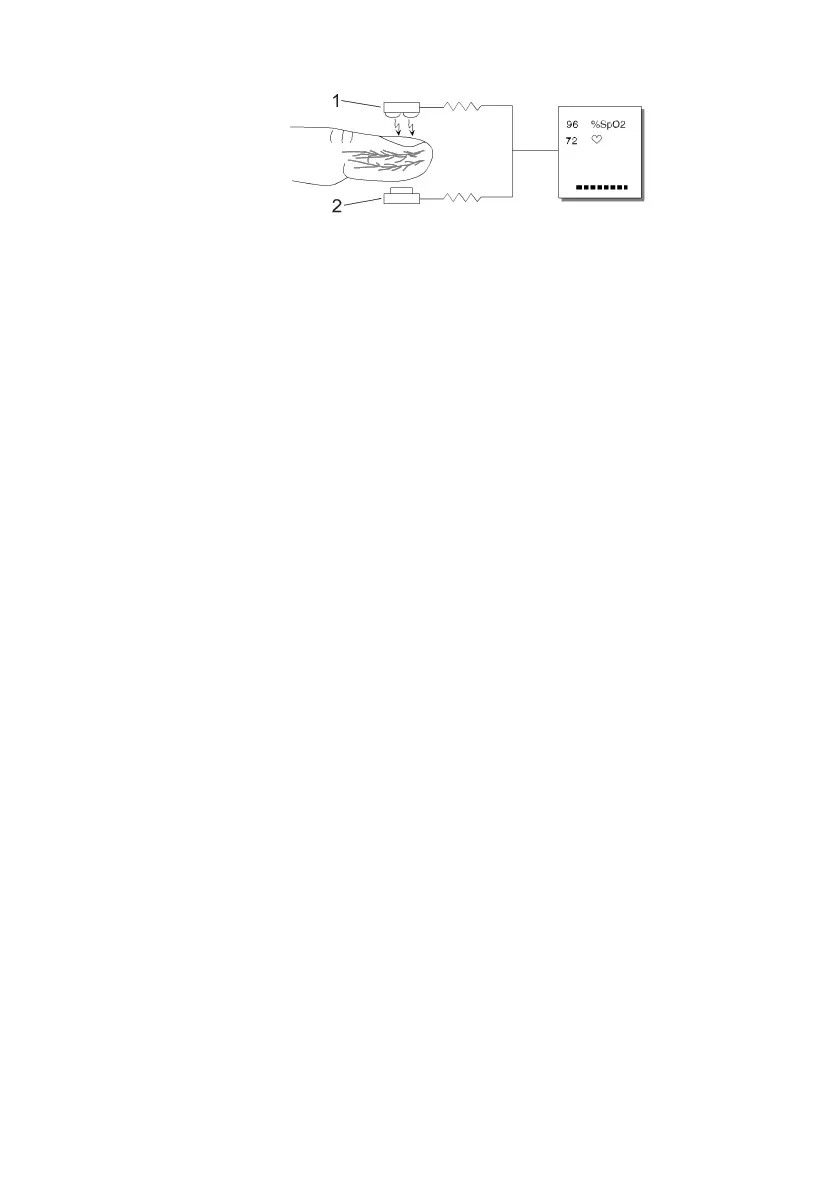
1
2
Figure 8.1: Theory of Operation
1. Low intensity Red and Infrared LED light sources
2. Detector
Oximetry processes these signals, separating the time invariant parameters
(tissue thickness, skin color, light intensity, and venous blood) from the time
variant parameters (arterial volume and SpO
2
) to identify the pulses and
calculate functional oxygen saturation. Oxygen saturation calculations can be
performed because blood saturated with oxygen predictably absorbs less red
light than oxygen-depleted blood.
WARNING!
Since measurement of SpO
2
depends on a pulsating vascular
bed, any condition that restricts blood flow, such as the use of
a blood pressure cuff or extremes in systemic vascular
resistance, may cause an inability to determine accurate SpO
2
and pulse rate readings.
WARNING! Under certain clinical conditions, pulse oximeters may display
dashes if unable to display SpO
2
and/or pulse rate values.
Under these conditions, pulse oximeters may also display
erroneous values. These conditions include, but are not limited
to: patient motion, low perfusion, cardiac arrhythmias, high or
low pulse rates or a combination of the above conditions.
Failure of the clinician to recognize the effects of these
conditions on pulse oximeter readings may result in patient
injury.
8.4 Attaching the Patient
WARNING! Prolonged use or the patient's condition may require changing
the sensor site periodically. Change the sensor site and check
skin integrity, circulatory status, and correct alignment at least
every 4 hours.
WARNING! When attaching sensors with Microfoam tape, do not stretch
the tape or attach the tape too tightly. Tape applied too tightly
 Loading...
Loading...