1
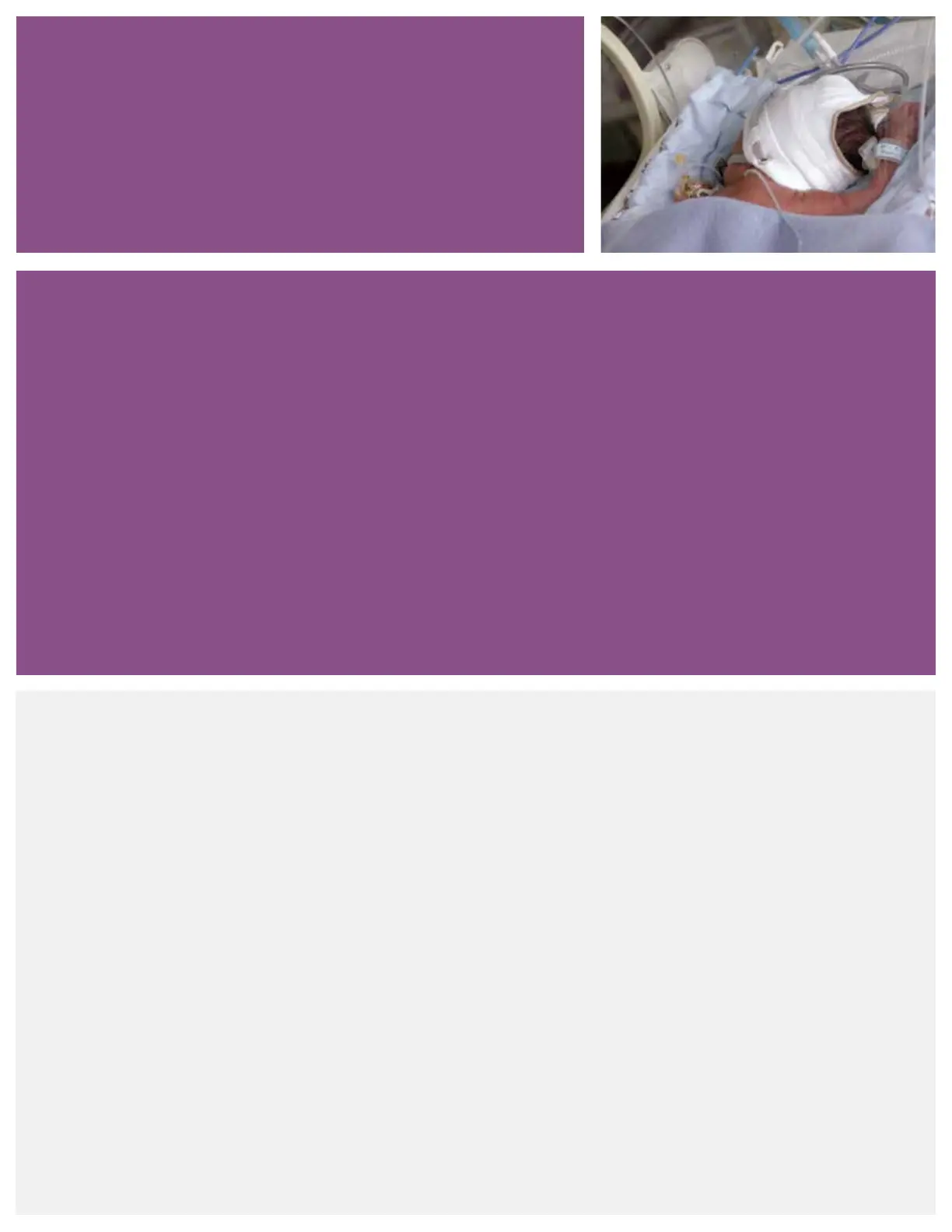
Infant nasal CPAP
Introduction
Worldwide each year, approximately 15 million (1 out of every 10) babies are born prematurely.
1
Premature or
low-birth weight (LBW) infants are at a high risk for respiratory problems due to underdeveloped lungs. Common
neonatal respiratory conditions include apnea of prematurity, respiratory distress syndrome, transient tachypnea
of the newborn (TTN), meconium aspiration syndrome, pulmonary edema and post-extubation support. These
conditions are often associated with decreased pulmonary compliance and functional residual capacity (FRC).
1,2
Several of these infants will require respiratory support.
Respiratory distress syndrome (RDS) is a condition that strains normal respiration due to the lack of natural
surfactant production. Approximately 50% of neonates born at 26 to 28 weeks gestation and 30% of neonates
born at 30 to 31 weeks gestation develop RDS.
2
What is surfactant?
Surfactant is a phospholipid, which reduces surface tension
to increase lung compliance.
Artificial surfactant may be given to help reduce surface
tension, increase compliance and improve ventilation.
Without additional respiratory assistance, many infants have
difficulty establishing the adequate functional residual
capacity (FRC) required to maintain normal respiration.
Respiratory support
Several options are available to help the clinician provide
respiratory support to the neonatal patient. Historically, the
initial treatment for infants with respiratory problems was
mechanical ventilation via an artificial airway. Intubation
presents a variety of challenges for any patient but
compounds problems with premature infants. Given the
potential complications of intubation, many physicians opt
for a less invasive approach for spontaneously breathing
infants that utilizes continuous positive airway pressure
(CPAP). As infants are preferential nose-breathers, nasal
CPAP (nCPAP) is the preferred method for treatment
delivery. CPAP enhances alveolar recruitment decreasing
pulmonary vascular resistance and intrapulmonary shunting,
stabilizes FRC and improves oxygenation. By increasing
surface area to alveolar gas exchange, CPAP decreases V/Q
mismatch. The goal of CPAP therapy is to maintain normal
lung volumes and oxygenation, while enabling the infant
to breathe on their own.
3,4
Physiologic effects of CPAP are
represented in the organizational chart on page 2.
CPAP overview
 Loading...
Loading...