Indications for use
2–5
• Abnormalities on physical examination
- Increased WOB
- Increased respiratory rate
- Intercostal and substernal recession
- Grunting and nasal aring
- Pale skin color
- Restlessness
• Deteriorating arterial/capillary blood gas values
(e.g., hypercapnea)
• Increased oxygen requirements to maintain a SaO
2
greater than 92% with FiO
2
> 60%
• Atelectasis and inltration
• Clinical conditions
- Apnea of prematurity
- Chest infections (e.g., pneumonia)
- Transient tachypnea of the newborn (TTN)
- Mild meconium aspiration
• Weaning/Post-extubation support
Contraindications for use
2–5
• Severe cardiovascular instability
• Respiratory failure dened as pH < 7.25 and
PaCO
2
> 60 mmHg torr
• Congenital malformations of the upper airway (cleft
palate, choanal atresia or tracheoesophageal stula)
• Congenital diaphragmatic hernia or untreated
bowel obstruction
• Poor respiratory drive unresponsive to CPAP therapy
(frequent apnea episodes associated with oxygen
desaturation and/or bradycardia)
What is work of breathing?
WOB describes the amount of effort required to breathe.
Any therapy that introduces incoming pressure to a
patient’s respiratory system potentially adds imposed
WOB. Infants with RDS experience elevated WOB levels,
and by expending additional effort to inhale and exhale
against pressurized gas, the infant consumes precious
calories overcoming the high WOB level. These calories
could otherwise be spent on vital recovery and growth
processes. In addition to helping the infant conserve energy,
a WOB reduction may reduce stress and anxiety levels.
3
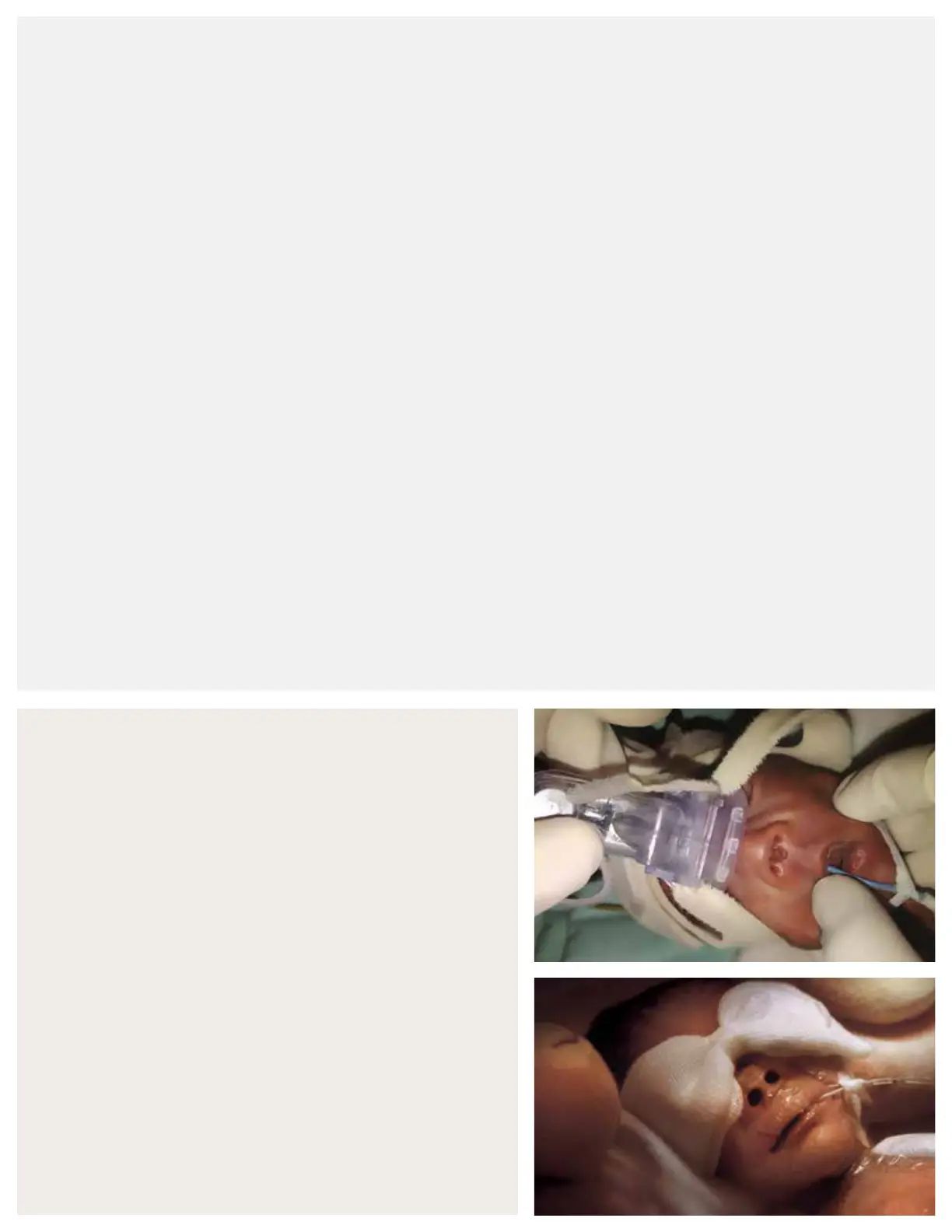
Columella necrosis
Nasal dilation
Potential problems associated with CPAP therapy
3,5,6
Clinicians should be aware of the possible hazards and
complications associated with CPAP, and take the
necessary precautions to ensure safe and effective
applications, such as:
• Possible loss of prescribed pressure and decreased FiO
2
due to mouth breathing
• Increased intrathoracic pressure reducing venous return,
which may lower cardiac output
• Barotrauma leading to surgical emphysema/
pneumothoraces
• Aspiration
• Deterioration in the respiratory condition, requiring
immediate ventilation
• Patient discomfort from prong/mask intolerance
• Nasal septal injury (e.g., columella necrosis)
• Blanching of the nares
• Dry mouth and airways
• Gastric ination
 Loading...
Loading...