RETeval Complete Option
RET
eval
Device User Manual 40
ambient light level is approximated by taking the geometric mean of the light level measured
inside the integrating sphere (ganzfeld) by a photodiode with an ambient light optical filter
bonded onto it.
Many of the protocols have constant retinal illuminance, which are described by the Troland unit
(Td). These protocols are identified with “Td” in the user interface and PDF reports. In these
protocols, the RET
eval
device measures the pupil size in real time and continuously adjusts the
flash luminance to deliver the desired amount of light into the eye regardless of the size of the
pupil according to the following formula: Troland = (pupil area in mm
2
) (luminance in cd/m
2
).
Thus, pupils do not need to be dilated to achieve consistent results. Even when using mydriatics,
people dilate to different diameters and results can be made more consistent by using the
Troland-based stimuli. While Troland-based tests make results less dependent on pupil size,
secondary factors such as the Stiles-Crawford effect and/or changes in the distribution of light
on the retina prevent Troland-based tests from being completely independent of pupil size (Kato
et al. 2015, Davis, Kraszewska, and Manning 2017, Sugawara et al. 2020). The built-in ISCEV
Troland protocols attempt to match the ISCEV candela protocols by assuming a 6 mm pupil
diameter (28.3 mm
2
pupil area). For example, the Troland equivalent to the dark adapted 3.0
ERG, which has a flash luminance of 3 cd∙s/m
2
, has a stimulus of (3 cd∙s/m
2
)(28.3 mm
2
) = 85 Td·s.
If the pupil diameter is 6 mm, the 85 Td·s stimulus will be the same as a 3 cd∙s/m
2
stimulus and
the resulting ERGs will therefore be the same.
There are cases where the stimulus compensating for pupil size may be inconvenient. These
protocols are identified with “cd” in the user interface and PDF reports. For example, the patient
cannot keep their eyelids sufficiently open for the device to measure the pupil, there is a desire
to stimulate the eye through a closed eyelid, or there is a desire to match the stimulus of a
previous publication. When looking for the presence of any retinal function, a bright constant
luminance stimulus may be sufficient.
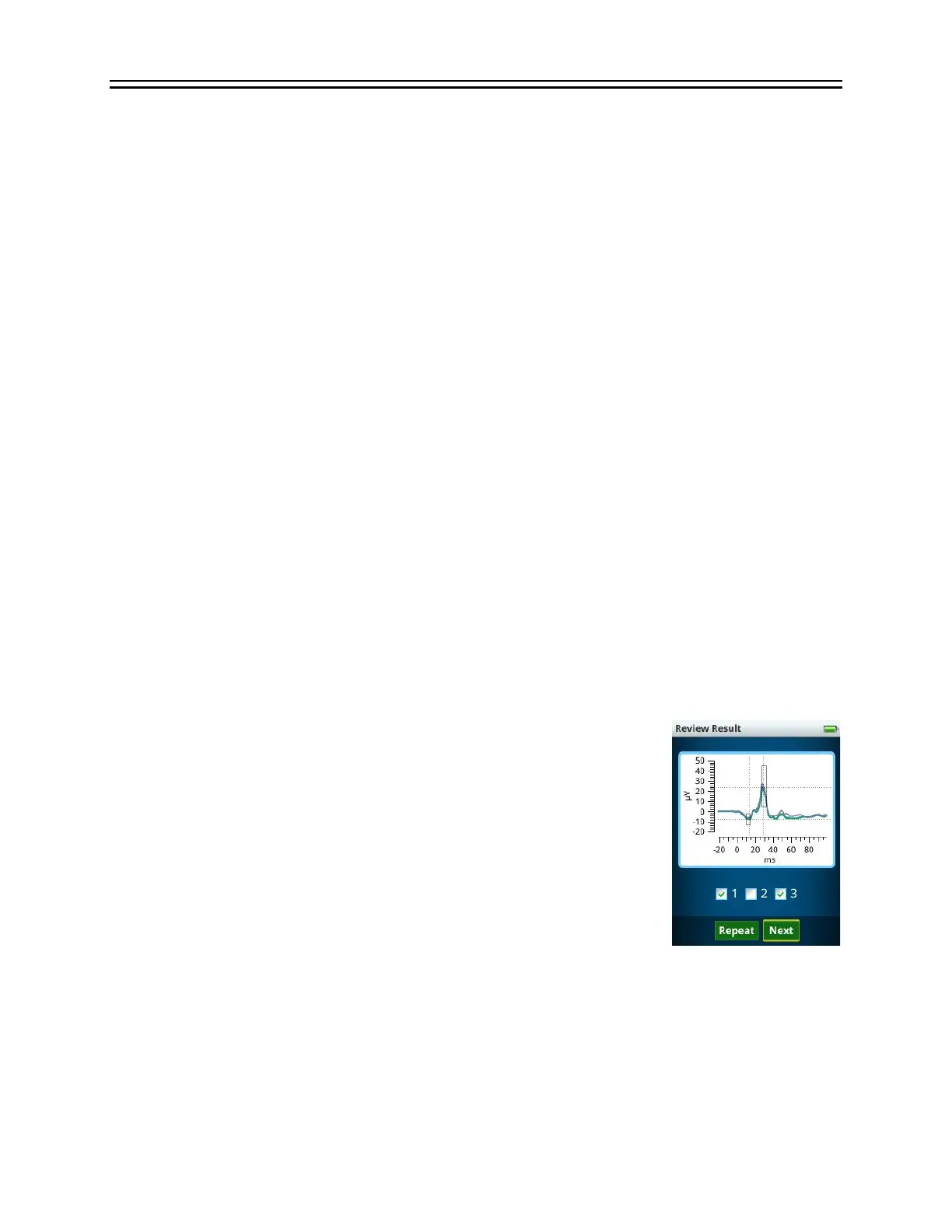
Subtests in protocols display the waveform results after each
measurement period and enable the operator to repeat the step as many
times as desired. Automated cursor placements are computed to the
average cursor placement across all repetitions. Any subtest can be
skipped without affecting the rest of the protocol. On the review screen,
the operator has the option of selecting which replicates to keep from
the reports. This option enables replicates to be deleted in the event,
for example, of poor patient compliance or excess noise in some
replicates. To remove a replicate, simply uncheck the box associated
with that replicate. Replicates can be selected or removed anytime while
collecting replicates. After you have moved to the next test step, you no
longer can alter the replicate selection for previous steps. When reference intervals are available,
a rectangular box is shown that encloses 95% of the data in the visually-normal test population.
Cursor measurements outside the rectangular box are therefore atypical. Atypical
measurements associated with disease (long times or small amplitudes) are highlighted in red
(i.e., < 2.5% for amplitudes or > 97.5% for times). Measurements close to the border of being
highlighted red (the next 2.5%), are highlighted in yellow. See the Reference Intervals section
in the manual (starting on page 67) for further details.
 Loading...
Loading...