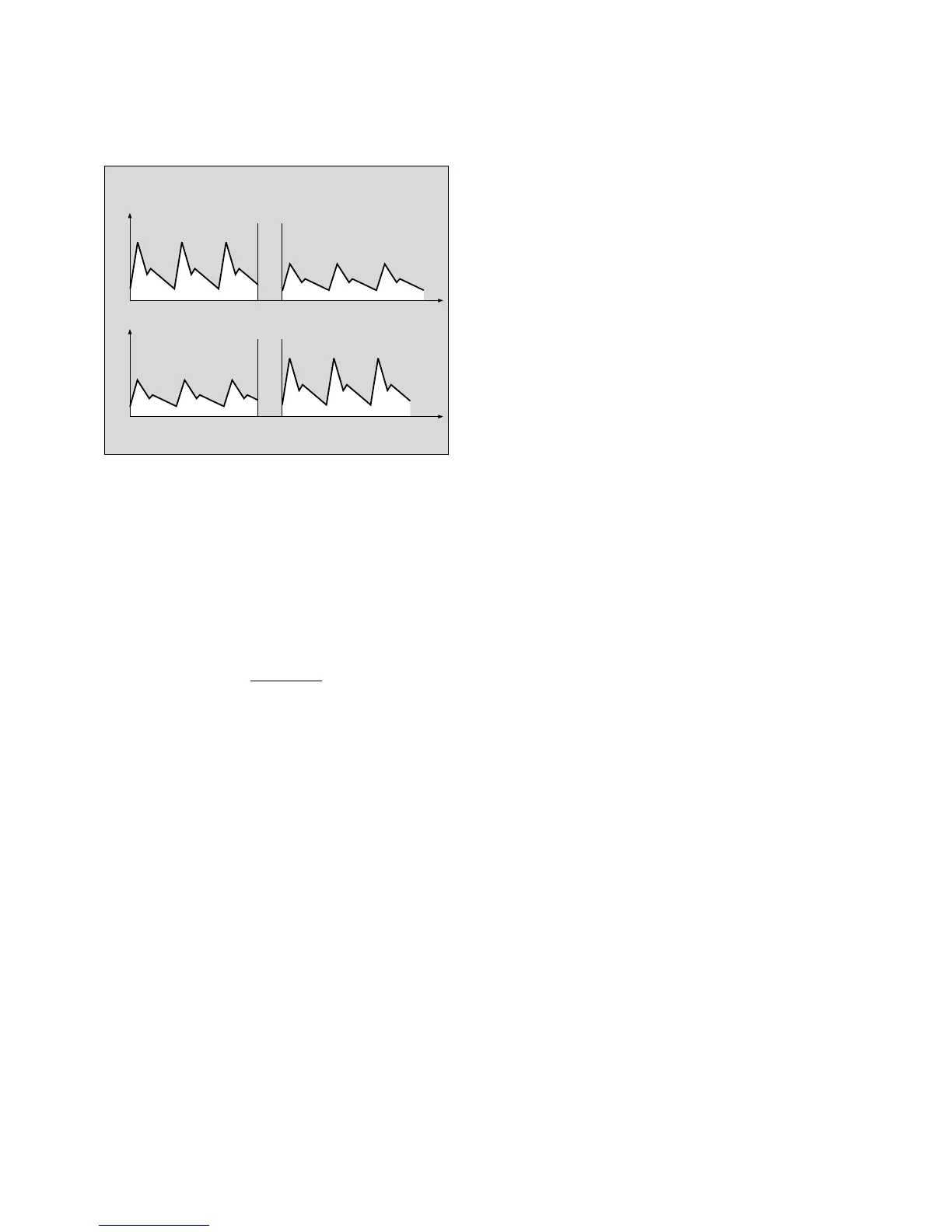
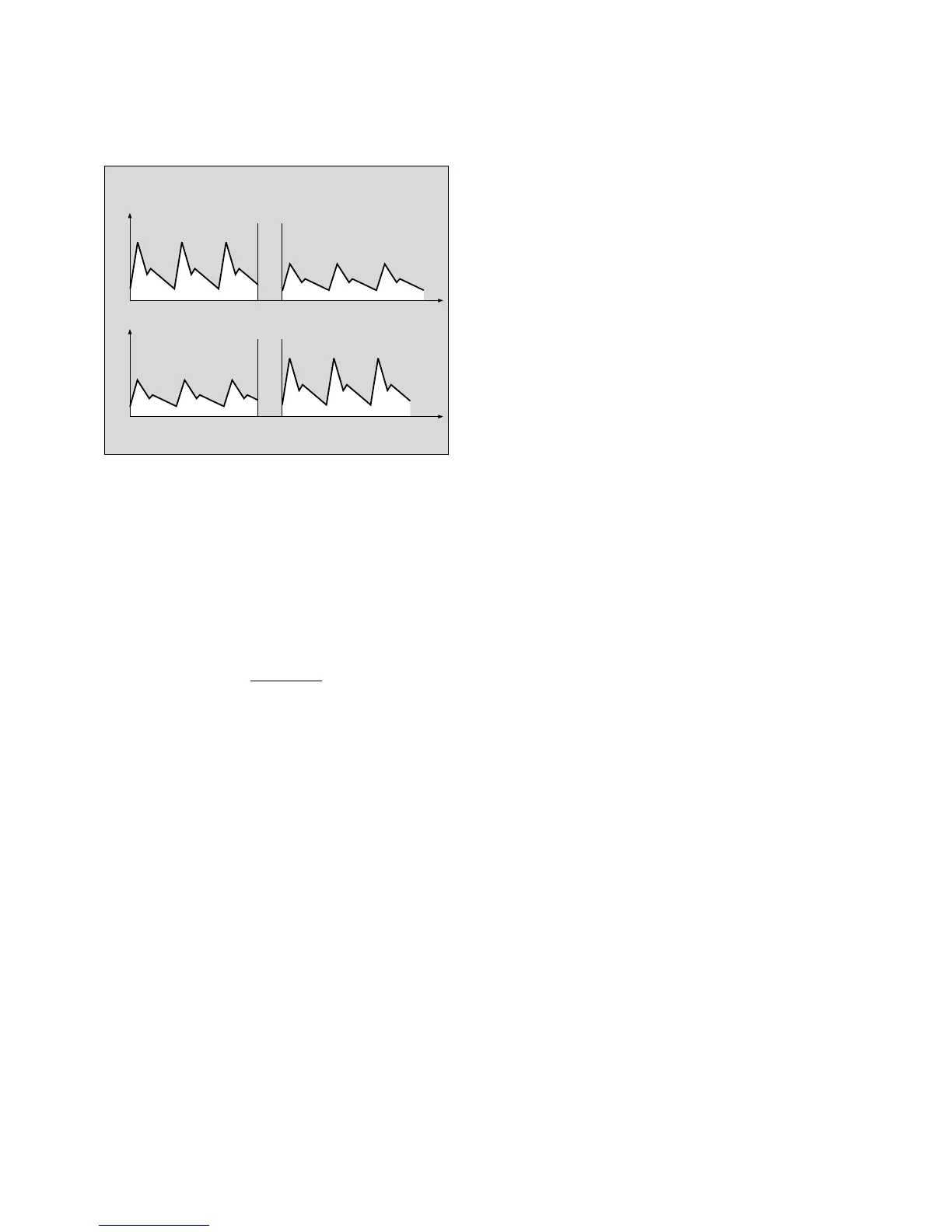
The diagram above shows an example of the light absor-
bed by the blood at 660 nm (red) and 920 nm (infrared).
At 660 nm, the absorption and corresponding pulse
amplitude decrease with increasing O2 saturation, but
rise at 920 nm. Since the absorption coefficients of
HbO2 and Hb are known for both wavelengths, the
system can calculate how much of these two haemo-
globins is present. The quotient obtained by dividing the
oxygenated haemoglobin (HbO2) by the reduced and
oxygenated haemoglobin (Hb + HbO2) is known as the
functional saturation:
% SpO2 (func) = 100
•
and refers to the haemoglobin capable of transporting
oxygen.
Dyshaemoglobins, HbCO and MetHb are normally
negligible, but may affect the accuracy of the measure-
ment.
Temperature measurement
Temperature-dependent change in resistance of an
NTC resistor (NTC = negative temperature coefficient)
with linearization circuit.
Pressure measurement
Principles of measurement:
Piezoresistive change of resistance in a membrane.
Determination of PEEP and plateau pressure:
PEEP (positive end-expiratory pressure) is the airway
pressure at the end of expiration.
Plat (plateau pressure) is the airway pressure measured
16 milliseconds before expiration begins.
Descriptions
Principles of measurement
Definitions for »low-flow« and »minimal flow« anaesthesia
132
Definitions for »low-flow« and »minimal flow«
anaesthesia
Low-flow anaesthesia is performed with a fresh gas flow
considerably below the minute ventilation. When setting
such low fresh gas volumes, the anaesthetic gases must
be returned to the patient via a semi-closed or closed
rebreathing system.
The rebreathing volume increases when the fresh gas
flow is reduced and the excess gas volume decreases
correspondingly.
Although the fresh gas flow can only be infinitely reduced
to the gas volume taken up by the patient at a given
moment of anaesthesia in a completely hermetic system,
a distinction is nevertheless made between the following
methods:
The fresh gas flow is reduced to 1 L/min for low-flow
anaesthesia and to 0.5 L/min for minimal-flow
anaesthesia.
In the case of non-quantitative anaesthesia in a closed
system, the gas delivery settings are corrected frequently
to adjust the fresh gas volume in line with the volume of
gas taken up by the patient so that the internal pressure
and charge of the breathing system do not decrease and
the ventilation pattern remains unchanged.
In the case of quantitative anaesthesia in a closed
system, the composition of the fresh gas corresponds
exactly to the volumes of oxygen, nitrous oxide and
inhalation anaesthetic taken up by the patient at a given
moment in anaesthesia. This ensures that the composition
of the anaesthetic gas also remains constant, in addition
to the gas charge in the system and the ventilation pattern.
(Source: Baum, J.: »Die Inhalationsnarkose mit niedrigem
Frischgasflow« (Inhalation anaesthesia with low fresh gas
flow), published by Thieme, Stuttgart 1992)
HbO
2
HbO2 + Hb
Pulse amplitude
Time (s)
at 660 nm red
O
2 saturation 100% O2 saturation
at 920 nm infrared
Pulse amplitude
Time (s)
08428971

 Loading...
Loading...