Müse Parameter Descriptions
230
CAEAthena
PN: 905K520652 v2.8
Chest Compression Efficacy
The Chest Compression Efficacy parameter is used to determine the effectiveness of chest
compressions administered by the caregiver. The 100% setting indicates that chest compressions are
completely effective, while the 0% setting prevents them from having any effect on intrathoracic
pressure.
Default: 100%
Options: 100%
0%
Tamponade Volume
The Tamponade Volume parameter is used to set the amount of fluid or blood that is building up in
the space between the myocardium and the pericardium, causing a cardiac tamponade.
Default: 0 mL
Range: 0 mL - 500 mL
Ischemic Index Sensitivity
The Ischemic Index Sensitivity parameter determines the relative sensitivity of the simulated
patient to myocardial ischemia. A lower ischemic index sensitivity value corresponds to less
sensitivity to an unfavorable oxygen supply/demand ratio (i.e., poor oxygenation with high heart
rate). A patient with a low value is less sensitive to poor oxygenation, takes longer to go into the
“death spiral” and, therefore, survives longer.
Default: 0.45
Range: 0.10 - 5.00
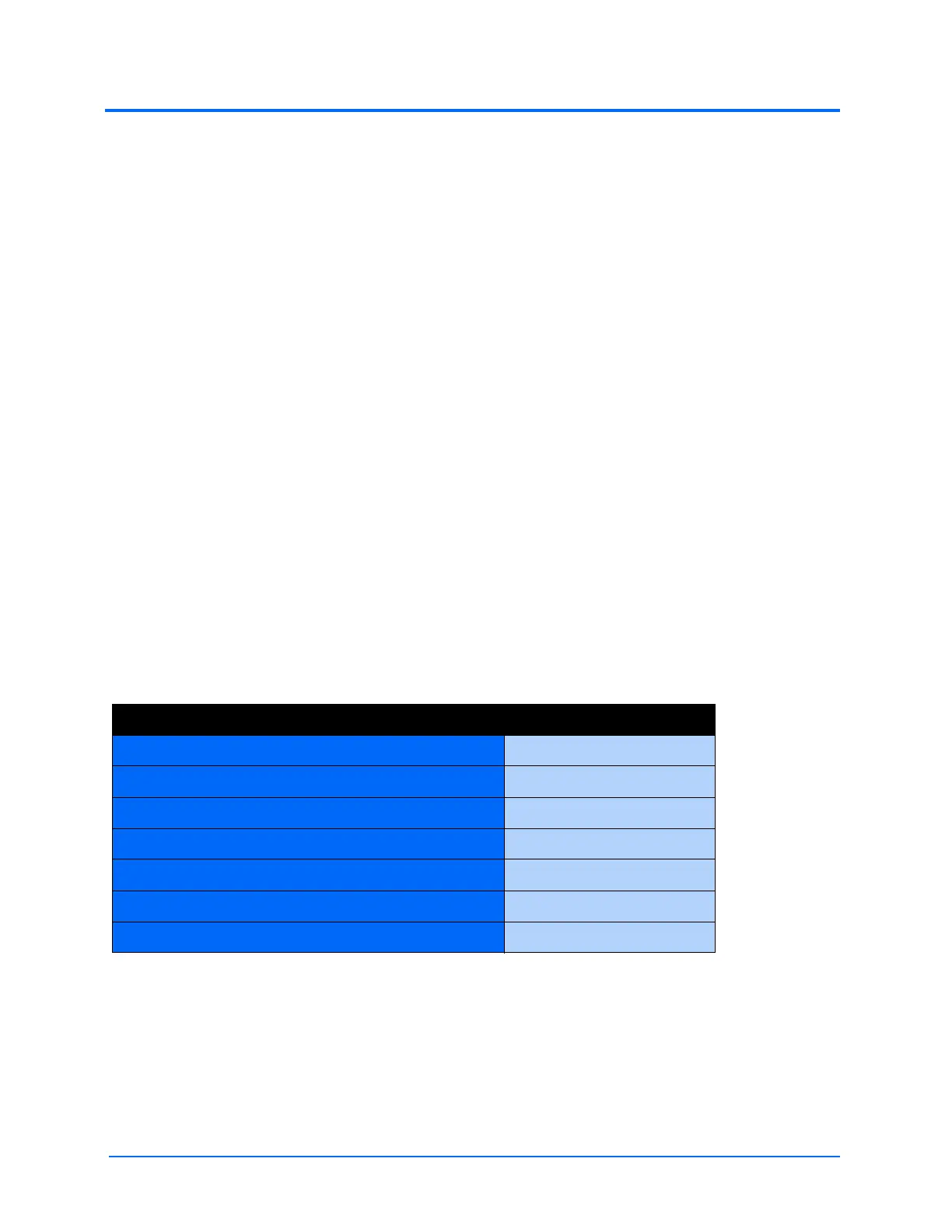
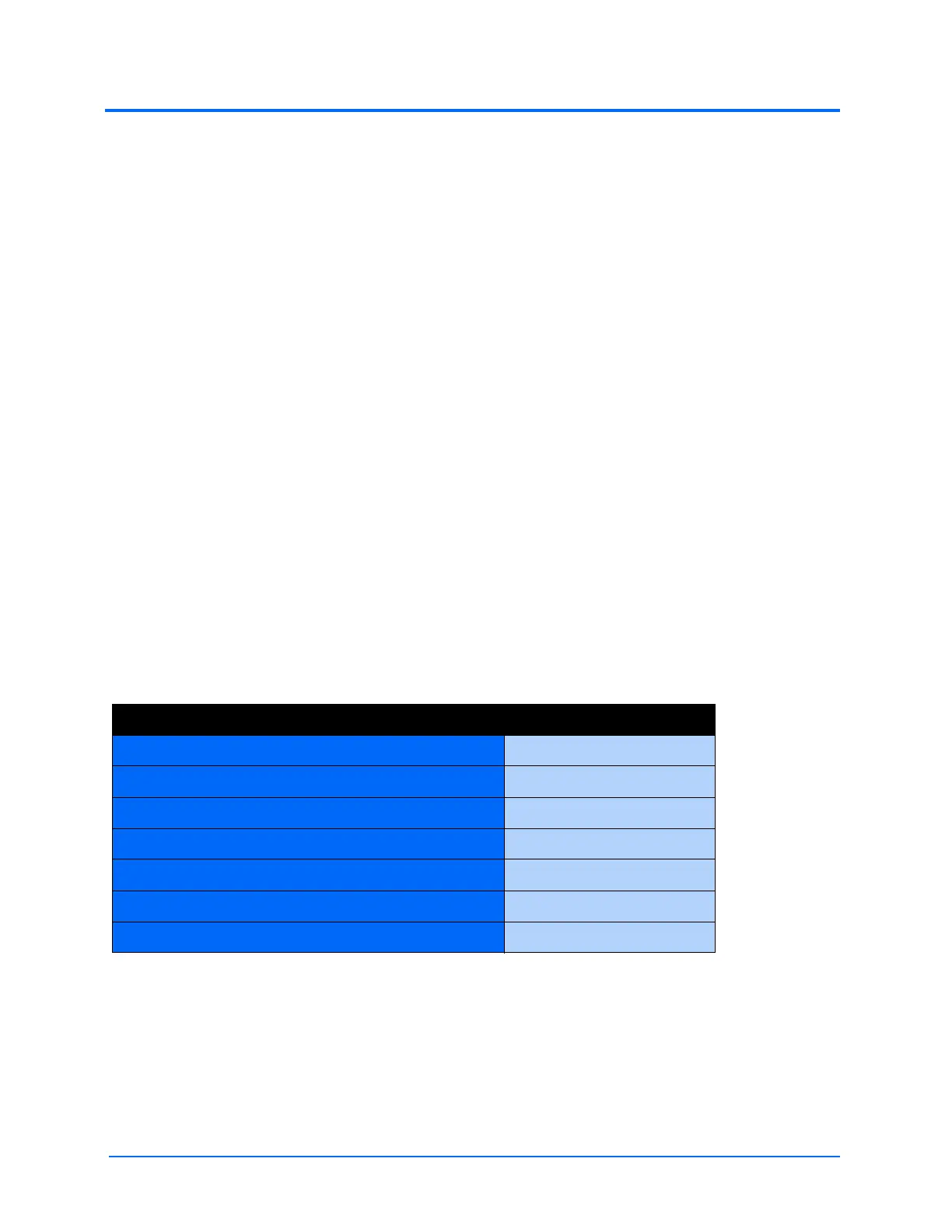
The patient’s response to myocardial ischemia may be altered using the Ischemic Index Sensitivity
parameter found on the Cardiovascular view. To make the patient less sensitive to ischemia, lower
the value below the default setting. To make the patient more sensitive, increase the value above the
default setting. These changes are then reflected in the patient’s Ischemic Index, as shown in the
table above.
Model-Driven ECG Rhythm Ischemic Index (I.I.)
Normal Sinus Rhythm (NSR) I.I. ≥ 0.90
Mild ST Segment Depression 0.90 > I.I. ≥ 0.70
Moderate ST Segment Depression 0.70 > I.I. ≥ 0.60
Premature Ventricular Contractions (PVCs) 0.60 > I.I. ≥ 0.40
Ventricular Tachycardia (VTach) 0.40 > I.I.
Ventricular Fibrillation (VFib) 1 minute after VTach
Asystole 1 minute after VFib

 Loading...
Loading...